HEALTH AND FITNESS
Behavioral Health Billing: Common Challenges and How to Overcome Them
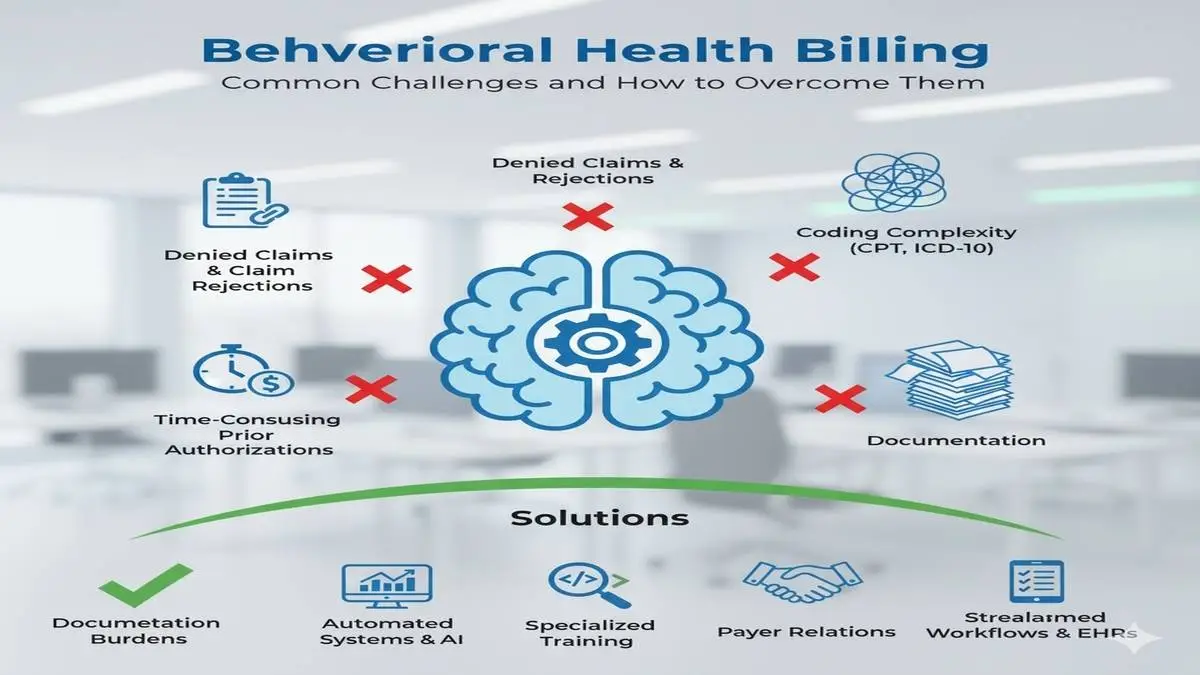
Healthcare billing processes are complicated and frustrating. In mental health and addiction care, billing becomes even more frustrating and complex due to complicated, changing insurer rules. Many practices, treatment centers, and behavioral health providers trying to maintain healthy, efficient financial systems hit significant obstacles. For this reason, Behavioral Health Billing is an area of focus for anyone in the field. The more providers understand the most common challenges and the most effective ways to remedy those challenges, the more they are able to preserve their revenue and relieve stress, helping their clinicians to attend to patient care rather than paperwork.
Table of Contents
Why Behavioral Health Billing Requires Special Attention
Behavioral Health Services are markedly different from any other area of health care. Unlike traditional practices, where predictable insurance processing and standard billing codes are the norm, behavioral health providers are required to contend with peculiar billing codes, rapidly changing payer rules, and differing documentation needs for each patient. Such system complexity greatly increases the chances of billing errors and resulting claim denials and payment delays.
The administrative responsibilities become even more complex with mental health and addiction services due to the extended durations of care. A patient may be under care for weeks, months, and even years. Consequently, a provider must monitor and manage a patient’s multiple claims throughout the revenue cycle. Given that the administrative workload increases, the need for well-organized systems and streamlined billing becomes even more important.
Insurance Verification and Eligibility Problems
The challenges a provider faces often begin even before the patient’s symptoms are addressed. For a behavioral health practitioner, insurance coverage and pre-authorization can be a prolonged and complex undertaking. Many practices in the behavioral health specialty have to deal with patients and families that have ambiguous mental health coverage benefits, and it is common to find plans that are particularly complex and ambiguous with respect to mental health coverage.
If a provider attempts to skip the verification process or rushes through it, the result is more often than not a denied claim. These denials result in wasted time and in time spent on appellant activities, which greatly exacerbate the administrative and financial burden of the practice. Establishing front-office procedures that include verification via the new HIT systems is a must. For health insurance verification systems, integrating various systems is more productive than systems that include only one level of automation. In most health insurance verification processes, narrowing down the parameters of the verification systems to a slotted funnel approach is the most effective.
The Different Challenges In Coding Behavioral Health Services
The next challenge is the coding system. Behavioral health uses different CPT and ICD-10 codes. Even the smallest mistake can lead to denial. As an example, therapy sessions require different modifiers depending on whether they are in person, virtual, or some combination. Different codes are used for certain addiction treatment programs, and those codes are not always easy for insurance companies to understand.
To provide effective support, billing departments will require additional training. Coders need to understand the practical implications of recent changes and how insurance companies will use those changes. Self-auditing will catch some mistakes prior to claim submission, but claim denial is an easier problem to troubleshoot with outsourcing. Specialized billing companies will ensure claims are coded properly for submission.
Timely Filing
From the different challenges involved in the billing process, timely filing can be the most difficult. The different payers will each have unique rules on when a claim is due. Missing a deadline will automatically trigger a denial. Practices that lack streamlined procedures are the most likely to struggle with these consequences.
Staying on top of deadlines and tracking workflows can eliminate problems before they start. Electronic tools for submitting claims can even save time and notify your practice when claims are ready for submission. Denial of claims is something that can always be avoided for future instances. Continuing a feedback loop creates a sustainable, efficient process.
Prior Authorization
Prior Authorizations for Behavioural health services are common. Especially for higher-level services, such as residential care or Partial Hospitalization Programs, prior authorization can prove frustrating to obtain. Authorizations can be time-consuming and frustrating for all parties involved, from providers to patients. Resolving this issue would require a dedicated staff member for authorizations. This role improves submission timing and ensures all necessary documents are ready. Relevant information should be provided to patients to maintain clear communication. Patients should be made aware that authorizations are part of the process and can ultimately affect treatment.
Managing long-term and ongoing care
Unlike a routine doctor visit, behavioral health treatment is typically a long-term process and is ongoing for a longer period of time. Patients may need to engage in weekly therapy, medication management, or attend structured programs that require several sessions over the course of months. Further, each session and each program should be documented, coded, and billed accordingly.
For billing departments, ongoing care means tracking multiple claims for long periods, which can lead to issues like duplicate billing and gaps in claim submission. To mitigate these situations, providers can use billing systems tailored for behavioral health care and comprehensive billing software. Systems of this kind enable staff to assess billing and coding for claims to ensure consistency and continuity, manage session tracking and interoperability, and update and align spreadsheets for ongoing care.
Patient Responsibility and Collections
Providers will also face issues with unsatisfied patient responsibility. Even with behavioral health services, bundled payments, and primary insurance, patients commonly pay a high percentage of fees because of copays, deductibles, and uncovered amounts. Risk of revenue leakage increases when these payments are poorly collected, which many practices underestimate.
To aid in collections, practices should communicate patients’ responsibilities alongside their financial responsibilities and cost estimates in excess of $100. Payment plans will help both parties, and staff trained in positive financial interactions will likely improve collection rates. Having a collection policy will help practices improve patient collections.
Technology Gaps and Manual Processes
Legacy technology can create problems for many behavioral health practices. Errors are more likely to happen in the revenue cycle and billing manual processes. Also, practices lacking integrated technologies can face challenges in communication across clinical and administrative staff, especially among billing departments.
Modern integrated automated billing practices resolve this issue. When clinical documents transition into billing, discrepancies and inconsistencies are less likely to happen. Providers can also obtain and use customizable reports to evaluate claims, denials, and overall revenue cycle performance. Appropriate technology investments and behavioral practices streamlining billing are a major part of resolving the problems.
Staff Training and Turnover
Billing is an administrative discipline and requires specific qualifications, and many practices also encounter an administrative position revolving door. Situations like incomplete or insufficient staff training also made behavioral health billing more convoluted, and mistakes proliferated.
Provider focus for this situation is staff training, and the instructions should center on consolidation and systematization in order to build up retention. Job improvement increases satisfaction along with accuracy. Also, standardized processes ensure consistency, even when the people on the team. Billing compliance can also be contracted to provide even more turnover stability. External partners provide greater expertise and experience in the discipline.
Compliance and Regulatory Changes
The healthcare industry undergoes constant changes, and so do the behavioral health providers. Changes in HIPAA regulations, payer requirements, and government program rules can impact billing. Compliance risks include the possibility of having claims denied and costly penalties.
Taking a proactive approach is the most effective way to manage compliance challenges. Providers can appoint compliance officers and contracting billing services that provide compliance updates and audits. Preparing your staff with frequent compliance audits and training will prepare them for inevitable changes. Incorporating a compliance focus will shield your practice from risks.
The Financial Impact of Denials
Each denial is a loss of revenue and a guaranteed loss in productivity. Denials in behavioral health billing, unfortunately, are a common industry loss. The longer a provider waits to address unresolved system issues, the more the practice and provider will lose.
Denial rates can improve when practices review and analyze billing patterns that reveal errors and areas in need of improvement. Billing staff should provide root cause resolution measures for coding, documentation, and eligibility issues, and for denial trends. Providers who manage denial trends will improve practice profitability and professional satisfaction.
How Outsourcing Solves Behavioral Health Billing Problems
For some practices, the answer to these persistent problems is outsourcing. Collaborating with billing specialists who concentrate on behavioral health offers the healthcare expertise, sophisticated technology, and systems that smaller practices can’t afford.
It also alleviates the pressure on clinical staff and guarantees that claims are submitted accurately and promptly. For providers, outsourcing offers real transparency through comprehensive reports and insights about the revenue cycle. With fewer claims denied and reimbursements speedier, practices have more time to concentrate on patient care.
Creating a Sustainable Future for Behavioral Health Practices
Billing challenges are, first and foremost, a question of sustainability. As demand for services continues to grow, the pressure on behavioral health providers is immense. With the right tools, practices can resolve financial challenges and maintain stability while continuing to provide vital care to the community.
When revenue cycles and billing systems function seamlessly, providers work with lower stress, patients receive care without interruption, and organizations improve their overall resilience. Creating a positive revenue cycle is about more than profitability. It’s about enabling clinicians to concentrate on what truly matters—and that is helping patients to heal.
Final Thoughts
Behavioral health has its challenges, and billing complexities are one of the most difficult challenges to deal with. Providers can forge the path to successful billing by integrating the right techniques with appropriate training and technology. Collaborating with billing professionals can validate that claims are correct, payments are received in the expected timeframe, and compliance has been completed. Indigo Billing is readily available to assist providers in the behavioral health industry to help remove stress and streamline complicated billing practices.
-

 GENERAL8 months ago
GENERAL8 months agoChristofle – For Those Who Dream of Family Heirloom Silver
-

 SPORTS10 months ago
SPORTS10 months agoDiscover the World of Football with Streameast: Watch Your Favorite Leagues and Tournaments
-

 GENERAL2 months ago
GENERAL2 months agoUncovering the World of кинокрадко: The Dark Side of Film Piracy
-

 GENERAL5 months ago
GENERAL5 months agoATFBooru: Anime, Gaming, and Subculture Imageboard























